Our DNA is under constant attack from many sources (chemicals and radiation, for example) that can result in genetic instability. This can lead to genetic disorders, chronic diseases and predisposition to cancer. Our bodies do their best to fight DNA damage, but it now seems their defensive response sometimes can cause more damage than good.
Researchers from Tel Aviv University recently found that elevated levels of ubiquilin-4, a protein that takes part in defending the genome from DNA damage, are actually harmful. They discovered that when the amount of ubiquilin-4 rises in tumor cells, the cells become more prone to genome instability, accelerating the tumor’s growth and making it resistant to some cancer treatments.
The discovery suggests that elevated ubiquilin-4 levels is a biomarker, or indicator, for genome instability.
“This novel biomarker provides new, critical information about the tumor stage and grade, as well as the patient’s chances of responding to treatment,” said lead researcher Prof. Yossi Shiloh. “Tumors with high levels of ubiquilin-4 may be more resistant to radiation and some chemotherapies than those with normal levels of this protein.
“But the good news is that they may also respond better to other types of cancer therapy. Obviously, this is vital information for clinicians and patients,” he adds.
Shiloh and his TAU team collaborated on the study with Prof. Christian Reinhardt of University Hospital Cologne and University of Cologne and Dr. Dave Hoon of the John Wayne Cancer Institute in Santa Monica, California. Their research was recently published in Cell.
The research shows that the body’s DNA damage response is key in maintaining genome stability in the face of harmful agents.
“There are so many proteins involved in responding to DNA damage, and behind every protein is a different gene. There are infinite ways in which a gene can mutate. Various combinations of these mutations may lead to chronic diseases and a predisposition to cancer, premature aging and other conditions,” explained Shiloh.
“We hope our findings will provide a new tool for tumor classification, prognosis and treatment design.”
(via Israel21c)
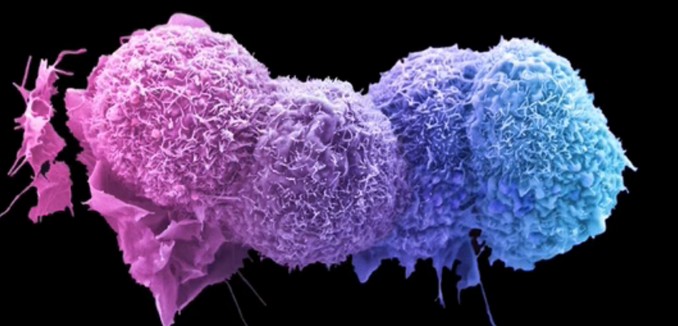
[Photo: Cancer Research UK / YouTube ]